Are federal dietary recommendations like the food pyramid responsible for our high rates of obesity?
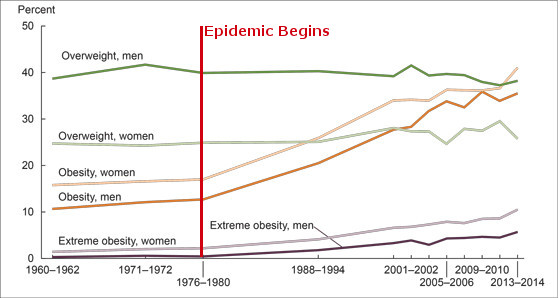
Obesity rates have been steadily increasing at an alarming rate, so these guidelines must have something to do with it, right?
We must analyze this suspicion critically and ask, are eating guidelines truly flawed and did they actually cause the obesity epidemic? Let’s find out!
What are the eating guidelines?
Various United States (U.S.) federal agencies provide guidelines around eating and nutrition as it relates to overall health. Below are the guidelines that were published in the 1970s:
- Don't consume excess calories
- Increase complex carbohydrates, including fruits, vegetables, and whole grains
- Reduce fat consumption from 40% to 30% of caloric intake
- Reduce saturated fat consumption to about 10% of caloric intake
- Getting up to 35% of your calories from fat
There are a few more recommendations addressing cholesterol and sodium, which seem out of date, but the most crucial aspects are quite reasonable.
The “Food Pyramid,” created by the USDA, is the most well-known eating guideline showing how much food a person should eat, with fats at the top of the pyramid as the smallest percentage and whole grains at the bottom of the pyramid as the largest percentage. The food pyramid was created in 1992, long after obesity rates started to rise. Trying to blame the obesity epidemic entirely on people following the food pyramid guidelines requires actual time travel.
Some have argued that the heavy emphasis on grains at the bottom of the pyramid was due to lobbying efforts from the agriculture industry. It is also true that its publication was paused from objections raised by meat and dairy lobbying groups and the design of the pyramid was modified to satisfy them (Nestle, 1993).
There are always financial and political incentives that distort science and policy, but it’s easy to forget that these issues come from many sides.
Does everyone follow these guidelines?
Nutritional guidelines don't directly change people's eating habits.
Government agencies have been heavily promoting eating more vegetables for a long time, and yet people still barely eat them. According to Lee et al. (2022), only 10% of adults eat enough vegetables. Krebs-Smith et al. (2010) found 80-90% of people exceed the guidelines for empty calories. There have also been studies looking into the effect of the guidelines on fat intake specifically, and they didn't change very much (Austin, 2011).
It's hard to argue that the dietary guidelines cause anything when people don't follow them in the first place!
But what if people followed the guidelines? Reidlinger (2015) tested if dietary guidelines were effective for cardiovascular disease risk. And it turns out that they are! When following the guidelines, people’s health improves and they tend to lose weight.
So, what really causes obesity?
Excess energy intake causes obesity.
The macronutrient distribution consumed is not relevant, as shown over and over again in research (Schwartz et al., 2017). Low-carb diets can work for weight loss, so can high-carb diets Seidelmann, 2018; Yang, 2022). Low-fat diets can help too, and more or less every other macronutrient permutation as long as it causes an energy deficit and people adhere to the diet.
Even though this is a straightforward explanation, this does not mean that ending the obesity epidemic is easy.
The factors that cause excess energy intake that may lead to obesity are complex, with a complicated interaction of genetic and environmental factors at play. The major factors include (but are not limited to) sedentary lifestyles from modern jobs, transportation, hyper-palatable foods, cheap food prices, food convenience, mental health problems, and more. We currently live in what has been called an “obesogenic environment” (Swinburn et al. 1999).
Here is a great (and complicated) system map by Vandenbroeck et al. from the Science Foresights Obesity Project created in 2006 that captures the complexity of the problem. The full model has 100+ variables and 300+ connections. And even that is simplified. You can see the graph in full resolution here.

Trying to address all these problems and inducing the needed behavioral changes for people to adhere to healthier habits is very difficult.
At the end of the day, it's still about calories in versus calories out, even if the internet and the world at large still want a macronutrient or food group scapegoat.
What can I do?
This isn't meant to say that high-fat diets are evil, nor that one should follow a high-carb diet. This is simply addressing the claim that dietary recommendations caused the obesity epidemic, which is factually wrong.
Addressing the obesity epidemic is incredibly difficult, but it's exponentially more difficult if we are trying to fix made-up causes.
If you need more help figuring out what nutritional strategy might work best for you, we recommend working with our one-on-one coaches. They can help you address the problems leading to excessive energy intake and make a plan tailored to you.
References
Lee, S. H., Moore, L. V., Park, S., Harris, D. M., & Blanck, H. M. (2022). Adults Meeting Fruit and Vegetable Intake Recommendations - United States, 2019. MMWR. Morbidity and mortality weekly report, 71(1), 1–9. https://doi.org/10.15585/mmwr.mm7101a1
Reidlinger, D. P., Darzi, J., Hall, W. L., Seed, P. T., Chowienczyk, P. J., Sanders, T. A., & Cardiovascular Disease Risk Reduction Study (CRESSIDA) investigators (2015). How effective are current dietary guidelines for cardiovascular disease prevention in healthy middle-aged and older men and women? A randomized controlled trial. The American journal of clinical nutrition, 101(5), 922–930. https://doi.org/10.3945/ajcn.114.097352
Schwartz, M. W., Seeley, R. J., Zeltser, L. M., Drewnowski, A., Ravussin, E., Redman, L. M., & Leibel, R. L. (2017). Obesity Pathogenesis: An Endocrine Society Scientific Statement. Endocrine reviews, 38(4), 267–296. https://doi.org/10.1210/er.2017-00111
Austin, G. L., Ogden, L. G., & Hill, J. O. (2011). Trends in carbohydrate, fat, and protein intakes and association with energy intake in normal-weight, overweight, and obese individuals: 1971-2006. The American journal of clinical nutrition, 93(4), 836–843. https://doi.org/10.3945/ajcn.110.000141
Ebbeling, C. B., Leidig, M. M., Feldman, H. A., Lovesky, M. M., & Ludwig, D. S. (2007). Effects of a low-glycemic load vs low-fat diet in obese young adults: a randomized trial. JAMA, 297(19), 2092–2102. https://doi.org/10.1001/jama.297.19.2092
Nestle M. (1993). Food lobbies, the food pyramid, and U.S. nutrition policy. International journal of health services : planning, administration, evaluation, 23(3), 483–496. https://doi.org/10.2190/32F2-2PFB-MEG7-8HPU
U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015 – 2020 Dietary Guidelines for Americans. 8th Edition. December 2015. Available at https://health.gov/our-work/food-nutrition/previous-dietary-guidelines/2015.
Yang, Q., Lang, X., Li, W., & Liang, Y. (2022). The effects of low-fat, high-carbohydrate diets vs. low-carbohydrate, high-fat diets on weight, blood pressure, serum liquids and blood glucose: a systematic review and meta-analysis. European journal of clinical nutrition, 76(1), 16–27. https://doi.org/10.1038/s41430-021-00927-0
Seidelmann, S. B., Claggett, B., Cheng, S., Henglin, M., Shah, A., Steffen, L. M., Folsom, A. R., Rimm, E. B., Willett, W. C., & Solomon, S. D. (2018). Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. The Lancet. Public health, 3(9), e419–e428. https://doi.org/10.1016/S2468-2667(18)30135-X
Swinburn, B., Egger, G., & Raza, F. (1999). Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive medicine, 29(6 Pt 1), 563–570. https://doi.org/10.1006/pmed.1999.0585